The term ‘single-use’ has appeared in many news and opinion articles over the last few years. Often considered to be a negative term – from an environmental standpoint – in the hospital space, its implications are quite different.
In 2021, for instance, a single use surgery retractor won The Queen’s Award for Innovation – being celebrated for its efficiency, usability, and ability to make surgeries safer. Compared to reusable retractors, single-use retractors are becoming far more popular, with hospitals up and down the US implicating them into their daily practices and improving operating room efficiency as a result. So how exactly do they do this?
Saving on Costs
It’s no secret that the healthcare system in the US is struggling. Rising costs and staffing shortages have put immense pressure on hospitals to find cost-effective solutions without compromising patient care, but finding these solutions is not easy – it’s important to find a balance, of course, between innovations that benefit healthcare practitioners without completely changing their routine.
Single-use retractors, while initially seeming more expensive due to their disposable nature, actually reduce expenses in the long-term. For one thing, they eliminate the need for sterilisation – which incurs costs for equipment and labour. Secondly, they don’t require an assistant to retract – reducing staffing cost and increasing workforce stability – and they are easily adjusted during surgery, which leads to a reduced operating time. Of course, reusable instruments do not have to be bought multiple times, but they also offer numerous false economies.
Inherent Concerns Surrounding Reusable Retractors
For reusable retractors in the operating room, there are multiple precautions that need to be adhered to – and yet still lead to many surgical instrument failures. Reusable instruments like this need to be maintained, stored, and used efficiently, but these concerns are ultimately exacerbated by reprocessing and sterilisation procedures.
A lot of the time, there is a lack of sinks to soak and rinse the instruments, ultrasonic cleaners are not used properly, inspection lamps or lenses are not used at all, and staff error leads to the manufacturer’s written instructions not being followed. With this in mind, the perceived cost saving for reusable retractors often comes to nothing, calling for a more simplified, economical alternative.
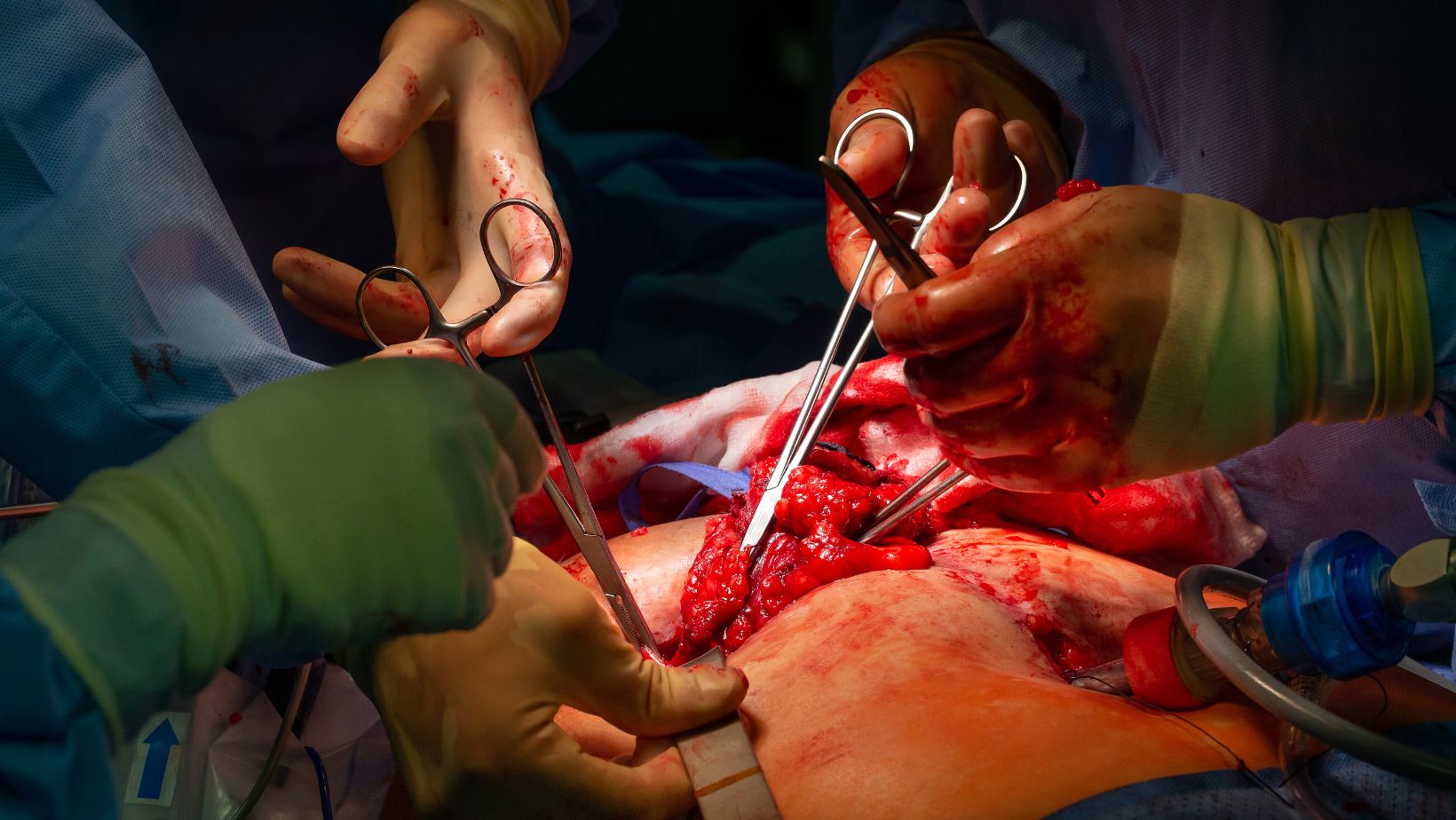
Playing a Crucial Role
While the cost-benefit is substantial, it’s important to remember the true benefactor of an innovation like this: the patient. Single-use retractors come sterile out of the packet, which essentially eliminates the risk of cross-contamination from improperly sterilized reusable instruments – as mentioned previously, simple staffing errors can drastically increase the chances of infection. They also have a consistent quality. For each procedure, the retractor is brand new, which means they are always in optimal condition – while reusable retractors degrade over time, which ultimately leads to inefficiencies.
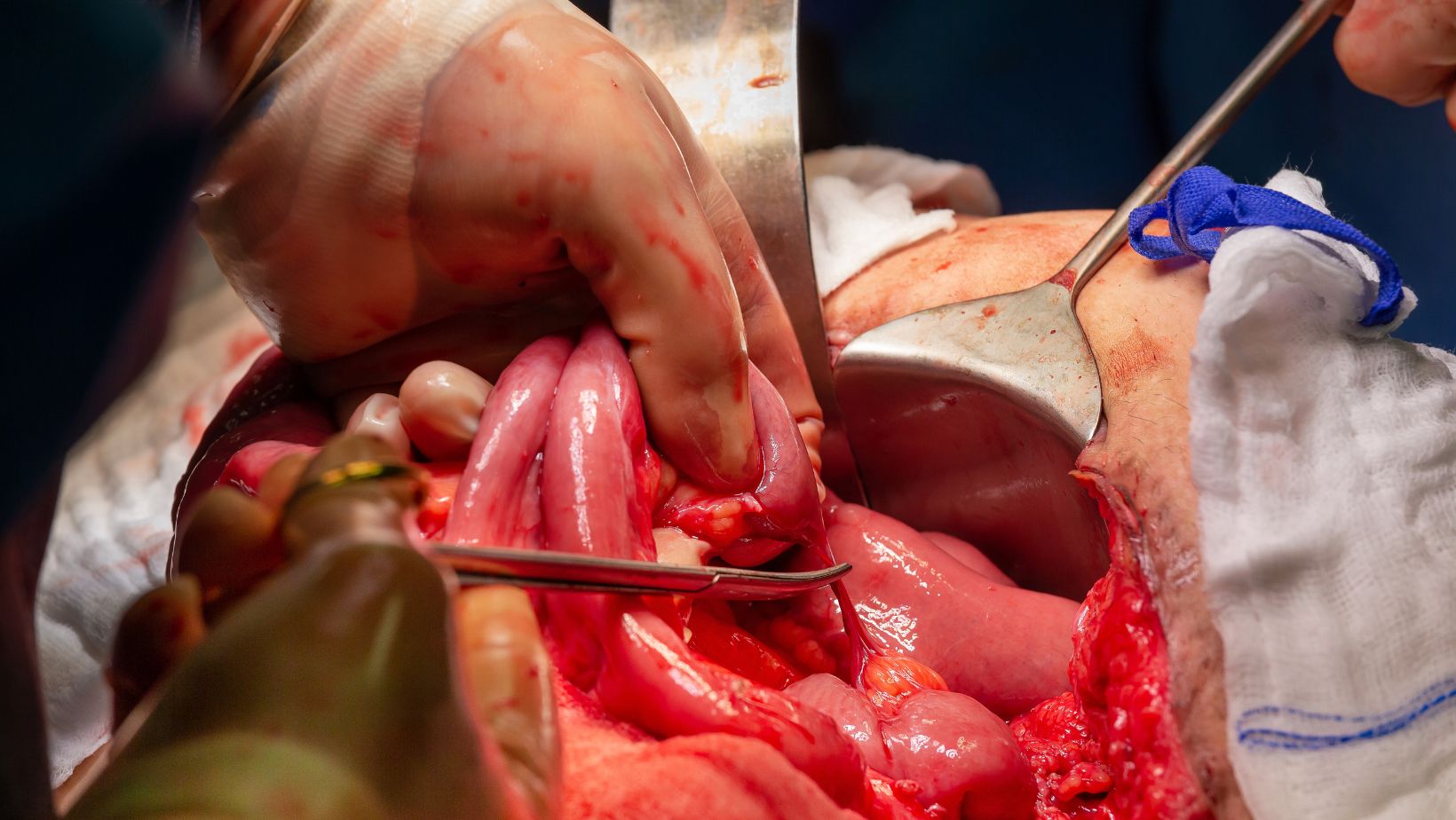
Complete with a more simplified inventory management – hospitals can streamline their inventory by reducing a large stock of reusable tools – and the allowance for quicker turnaround times between procedures – which enables more surgeries to be scheduled and performed in a day – single use retractors are revolutionising the surgical process, making them a key part of the healthcare industry’s hopeful rejuvenation over the next decade.

